Introduction:
When we think of tuberculosis, we often associate it with lung infections. However, did you know that tuberculosis can also affect other parts of the body, including the spine? Spine tuberculosis, also known as Pott's disease, is a severe but treatable condition that affects the bones in the spine. In this blog, we will discuss what spine tuberculosis is, its causes, symptoms, diagnosis, and treatment options, all in simple terms that anyone can understand.
What is Spine Tuberculosis?
Spine tuberculosis is a bacterial infection caused by Mycobacterium tuberculosis that affects the vertebrae (bones) of the spine. It is usually transmitted from an active tuberculosis infection elsewhere in the body through the bloodstream or lymphatic system. The infection can cause the affected vertebrae to weaken and collapse, leading to pain, deformity, and other complications.
Causes:
The primary cause of spine tuberculosis is the bacteria Mycobacterium tuberculosis. It can be transmitted when someone with an active tuberculosis infection coughs or sneezes, releasing tiny infected droplets into the air. If these droplets are inhaled by another person, the bacteria can enter their body and spread throughout, potentially reaching the spine.
While anyone can potentially be affected, some individuals are more susceptible to the Spine Tuberculosis. Here are some common risk factors:
1. Weakened Immune System:
-people living with HIV/AIDS,
-undergoing chemotherapy,
- taking immunosuppressive medications
2. Close Contact with Active Tuberculosis Patients
3. Living in Overcrowded or Unsanitary Conditions
4. Malnutrition
5. Age and Gender: Children and older adults are more vulnerable.
6. History of Tuberculosis:
-Individuals who have had tuberculosis in the past. The bacteria can remain dormant in the body and reactivate later, targeting the spine.
7. Poor Overall Health:
-Chronic conditions, such as diabetes, kidney disease, or lung disease
Which bones of spine are most affected by tb?
Thoracic spine is the most frequently involved, tuberculosis can also affect the lumbar spine, cervical spine, and sacrum, although less commonly.
In spine tuberculosis, the infection typically starts in the intervertebral discs and the adjacent vertebral bones. Over time, the infection spreads to the vertebral bodies, leading to their destruction and collapse. In some cases, the infection may begin in the vertebral body itself or in the posterior part of the bony vertebral ring.
Spine tuberculosis can also extend to involve the spinal cord and its protective coverings, known as the meninges. This can result in additional complications and neurological symptoms.
 |
Symptoms:
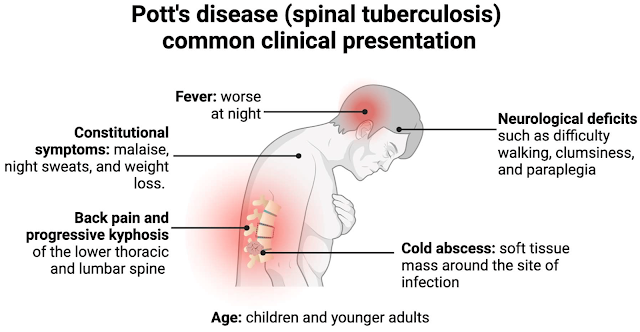
Spine tuberculosis can cause a variety of symptoms, which may include:
1. Persistent back pain, especially at night or with movement.
2. Stiffness and limitation of spinal movement.
3. Gradual loss of height or development of a hunchback deformity(Kyphosis).
4. Weakness or numbness in the legs or hands, loss of bladder-bowel control (Neurological compression)
5. Classic Symptoms of Tuberculosis like Fever, Fatigue, weight loss, and loss of appetite may or may not be seen
Spine Tuberculosis Diagnosis:
Patients with relevant symptoms and risk factors should be suspected of having spine tuberculosis. To confirm the diagnosis, the following tests are recommended:
1. X-ray: Shows disc height loss, vertebral collapse, and spinal deformity.
2. MRI Scan: Reveals detailed infection information, such as disc and vertebral body involvement, spinal cord compression, and treatment response. Contrast MRI is preferred. However, it cannot confirm tuberculosis alone; a biopsy is needed.
3. CT Scan: Provides detailed bony anatomy information like end plates status, pedicle & posterior bony elements integrity . It also assesses bone healing status in already under treatment patients.
4. Culture and Sensitivity: Determines the type of tuberculosis and guides medication selection based on bacterial response to different drugs.
5. Other tests:
-HRCT chest and sputum test to rule out lung infection
-Blood tests like CBC,ESR,CRP to assess infection severity and
progress.
-Tests to rule out other bacterial infections like Urine culture,
blood culture etc.
6. Biopsy: Essential for confirming the diagnosis and differentiating between infections and tumors. Also used for culture and sensitivity testing to determine effective antibiotics.
- CT Guided Biopsy: Retrieves material using a needle guided by CT imaging.
- Fluoroscopy Guided Biopsy: Collects target material using an intra-operative x-ray machine.
- Surgical Biopsy: Performed when other biopsy methods fail or are impractical.
7.GeneXpert/CBNAAT :
GENEXPERT is a diagnostic technology used for the detection of various infectious diseases, including tuberculosis (TB). It is a nucleic acid amplification test that detects the DNA of the bacteria causing TB, Mycobacterium tuberculosis.
It offers certain advantages in diagnosing TB, including spine tuberculosis:
1. Rapid results: Provides results within a few hours itself.
2. High sensitivity: high sensitivity in detecting M. tuberculosis DNA, even in samples with a low bacterial load
3. Simplicity: simple to perform and does not require extensive laboratory expertise. It can be used in settings with limited resources and in areas where skilled personnel are scarce.
To perform a GeneXpert test for spine tuberculosis, Tissue sample is obtained by biopsy from the affected part of Spine. The collected sample, such as a tissue biopsy or aspirate, is then processed and analyzed using the GeneXpert system.
DIFFERENTIAL DIAGNOSIS :
When considering tuberculosis (TB) of the spine, several other conditions which can present with similar symptoms and radiographic findings should be considered.
1. Pyogenic spondylodiscitis (PS): It is a bacterial infection of the spine, commonly caused by Staphylococcus aureus . It shares similar clinical features with TB spine, including back pain, fever, and localized tenderness. Differentiating between PS and TB spine often requires microbiological investigations, such as blood cultures or tissue biopsy, to identify the causative organism.
2. Brucellosis: A systemic bacterial infection caused by various species of Brucella. It can involve the spine, leading to brucellar spondylitis. The clinical presentation, including back pain, fever, and constitutional symptoms, can resemble TB spine. Serological tests, blood cultures, and imaging studies are used to differentiate brucellar spondylitis from TB spine.
3. Fungal infections: Fungal infections, such as histoplasmosis, coccidioidomycosis, or blastomycosis, can involve the spine and mimic TB spine. These infections are more prevalent in specific geographic regions and have different risk factors. Diagnosis often requires specialized fungal cultures, serological tests, or molecular diagnostic methods.
4. Metastatic cancer: Metastatic cancer to the spine can cause destructive lesions and compression fractures, similar to TB spine. A thorough evaluation with imaging studies, biopsy, and clinical correlation is essential to differentiate metastatic cancer from TB spine.
The below table shows difference between two common Spine infections:
|
Criteria |
Pyogenic Spondylodiscitis (PS) |
Tuberculous Spondylodiscitis (TS) |
|
Clinical Presentation |
Acute or subacute onset |
Insidious or chronic onset |
|
Severe back pain |
Back pain, constitutional symptoms
(fatigue, weight loss) |
|
|
Fever |
Night sweats |
|
|
Risk Factors |
Recent surgery |
History of exposure to
tuberculosis |
|
Invasive procedures |
Immunocompromised individuals
(e.g., HIV-positive) |
|
|
Urinary tract infections |
High tuberculosis prevalence in
the region |
|
|
Laboratory Findings |
Elevated CRP and ESR |
Elevated ESR, normal or mildly
elevated CRP |
|
Imaging Features |
Single vertebral level involvement |
Involvement of multiple adjacent
vertebral bodies (skip lesions) |
|
Pronounced endplate erosions |
Gradual involvement of entire disc
space |
|
|
Predilection for anterior
vertebral body |
No specific predilection for
vertebral body location |
|
|
Microbiological Investigations |
Blood cultures, pus cultures,
other source cultures |
Tissue sample for AFB staining,
culture, molecular tests |
|
(e.g., GeneXpert) for
Mycobacterium tuberculosis |
Treatment:
Fortunately, spine tuberculosis is treatable, but it requires a long-term commitment. Here is the overview of Spine TB management:
1. Medical Management:
- Initiate Weight based Anti-Tuberculosis Treatment(ATT) as soon as the biopsy/GeneXpert/Culture Reports are results are available as per Drug susceptibility. Do not Start empirical ATT without microbiological Confirmation !!
- Consult with an infectious disease specialist or pulmonologist for guidance on drug regimen selection and dosage if required. Your Spine Surgeon will take a call in this regard based on case to case.
- Typically, a four-drug regimen consisting of isoniazid, rifampicin, pyrazinamide, and ethambutol is used for the initial 2 months, followed by a continuation phase of isoniazid, rifampicin & ethambutol for a total treatment duration of 7-10 months.
- Monitor the patient closely for medication side effects and provide appropriate supportive care.
2. Medical Management in case of Drug-Resistance :
The medical management of drug-resistant spine tuberculosis (TB) can be challenging and requires a comprehensive approach.
Drug resistance in TB is commonly associated with resistance to one or more of the first-line anti-TB drugs, such as isoniazid and rifampicin.
In some cases, there may also be resistance to second-line drugs, making treatment even more complex.
1. Accurate Diagnosis: Accurate and timely diagnosis is crucial. Drug susceptibility testing (DST) should be performed to determine the drug resistance pattern, as this will guide the selection of appropriate medications.
2. Specialist Consultation: The management of drug-resistant spine tuberculosis should involve a team of specialists, including an infectious disease specialist or TB expert.
3. Drug Regimen Selection:
Based on the DST results, a personalized drug regimen should be formulated.
For drug-resistant TB, second-line anti-TB drugs are used, such as fluoroquinolones (e.g., moxifloxacin, levofloxacin), injectable agents (e.g., kanamycin, amikacin), and other drugs like ethionamide, para-aminosalicylic acid (PAS), linezolid, bedaquiline, and delamanid.
The choice of drugs will depend on the resistance pattern and individual patient factors.
4. Duration of Treatment: Treatment for drug-resistant spine TB is usually prolonged and can last anywhere from 18 to 24 months or more. The duration will depend on the severity of the infection and the response to treatment.
3. Surgical Management:
Consider surgical intervention in the following situations:
- Spinal instability
- Spinal Deformity
- Progressive neurological deficits
- Large Abscess formation
- Failure of medical treatment or drug resistance
- Need for a Open Biopsy
Discuss with your spine surgeon to determine the most appropriate surgical approach, such as decompression, stabilization, or abscess drainage.
Postoperative ATT should be continued as per the medical management guidelines despite of surgical management.
5. Supportive Care:
- Provide pain management through analgesics, physical therapy, and supportive orthotic devices.
- Monitor the patient's progress regularly through clinical evaluation, imaging, and laboratory tests.
- Encourage patient compliance with the full course of anti-tuberculosis medication.
- Promote proper nutrition and a healthy lifestyle to support the patient's overall well-being.
6. Follow-up and Monitoring:
- Schedule regular follow-up visits to assess treatment response, monitor for complications, and adjust medication as needed.
- Repeat imaging studies (X-ray, MRI, or CT scan) at appropriate intervals to evaluate treatment effectiveness and detect any disease progression or complications.
- Monitor liver function tests and other relevant laboratory parameters to identify potential medication-related adverse effects.
7.Patient Education:
- Educate patients about the importance of adherence to ATT, potential side effects, and the need for regular follow-up.
- Emphasize the necessity of maintaining good nutrition, rest, and hygiene for better recovery.
- Address any concerns or queries raised by the patient or their family members.
Conclusion:
Spine tuberculosis is a serious condition that can cause significant damage to the spine if left untreated. If you experience persistent back pain or other symptoms, consult a Fellowship Trained Spine Surgeon promptly. With early diagnosis and appropriate treatment, including medications and, if necessary, surgery, spine tuberculosis can be effectively managed, allowing you to regain your health and live a fulfilling life. Remember, knowledge and timely action are your best allies when it comes to your spinal health.


















Thanks for sharing valuable information about Spine. If you want to know more about the Best Doctor For Spine Surgery Click Here:- spine doctor in ahmedabad |
ReplyDeletespine surgeon in gujarat